There was a sense of foreboding outside room 527 that night at shift change. The unfortunate soul in that room had been in the hospital over a week with COVID-19 and had followed the pattern we had seen countless times. She had a severe case and was on a lot of oxygen but was holding her own without a lot of symptoms as long as she kept her oxygen on. Then, without warning, her blood work showed signs of rapidly increasing markers of inflammation and she started to look worse. She had escalating requirements for oxygen and was put on CPAP. The thing that was so scary to me as I started the shift that night was how she looked. She just looked so tired. She could not open her eyes or say even a few words. Her breathing was rapid and shallow and it didn’t appear she could last much longer. I adjusted her CPAP but over the next couple of hours, her oxygen levels started to drop. I had no choice but to put her on a ventilator.
The unspoken foreboding was palpable in the room. We all knew that when patients go on the ventilator things usually don’t turn out well. Most will not survive, many will have prolonged hospital courses with severe disabilities, few walk out of the hospital, and nobody is ever the same.
While this poor lady’s experience with COVID-19 was towards the extreme, how this pandemic has negatively impacted lives is myriad. One of the most common is the most annoying for some and crisis inducing for others. Of course, I speak of the dreaded quarantine. My home has been afflicted with this plague on multiple occasions straining the nerves of mother and child alike. For us, it was a great nuisance. For many, it can be an economic or childcare disaster. Throw in was the added cruelty that those in quarantine were imprisoned for longer than the infected individuals who put them there in the first place just for good measure. Two weeks can be a very long time.
With all that in mind, I was quite surprised to learn of new recommendations on quarantine from the CDC that came out this week.
Here’s the new recommendations:
I have rephrased these a bit to create simplicity, something the CDC seems to struggle with. I find their website to be the internet equivalent of waiting in line at the DMV, but I digress.
- The quarantine can end after Day 10 without testing and if no symptoms have been reported during daily monitoring.
- The quarantine can end after Day 7 if a diagnostic test is negative and if no symptoms were reported during daily monitoring. The specimen may be collected and tested within 48 hours before the time of planned quarantine discontinuation (e.g., in anticipation of testing delays), but quarantine cannot be discontinued earlier than after Day 7.
What was interesting is that the recommendations included an explicit mention of the risk of transmission in each case. It was 1-10% ending on day 10 and 5-12% on day 7 with a negative test.
The CDC does not mention it specifically, but I assume that the testing they are referring to is PCR testing and not rapid antigen testing. I assume this is based on the high false-negative rate of rapid antigen testing and the fact that they use a time of within 48 hours of planned quarantine discontinuation. The PCR test results come back around 48 hours (depending on the testing situation).
The original recommendations to quarantine for 14 days were based on the fact that it was rare for people to develop symptoms more than 14 days after their exposure.
The reason for the change came in some respect from new data modeling the risk of transmission taking into account the presence of a negative test. What was more interesting and perhaps more important, the changes come from an acknowledgment of how the burdens of quarantine can decrease the public’s compliance with the recommendations. They specifically mention three issues:
- The strain of quarantine on the physical, mental, and economic health of the quarantined individuals.
- The burden on public health systems and communities, especially during periods when new infections, and consequently the number of contacts needing to quarantine, are rapidly rising.
- A concern that the prospect of quarantine may dissuade recently diagnosed individuals from being forthright with contact tracers if they perceive the length of quarantine as onerous.
the changes come from an acknowledgment of how the burdens of quarantine can decrease the public’s compliance with the recommendations.
Wait, we can test out of quarantine now?
The new recommendations allow for shortening the quarantine from 10 to 7 days if a test collected on day 5 or after is negative. This was influenced by data modeling of the risk of transmission over time in quarantine (2 other models found similar results).
Remember, the purpose of quarantine is to see how long after infection someone infected with SARS CoV-2 can transmit the virus. The dark blue bar is quarantine plus a negative test, the light blue is without the negative test. The little narrow black bars on top show you the range that the numbers could fall into. In other words, the risk of transmission falls somewhere between the top and bottom of the narrow bars. Notice a few things:
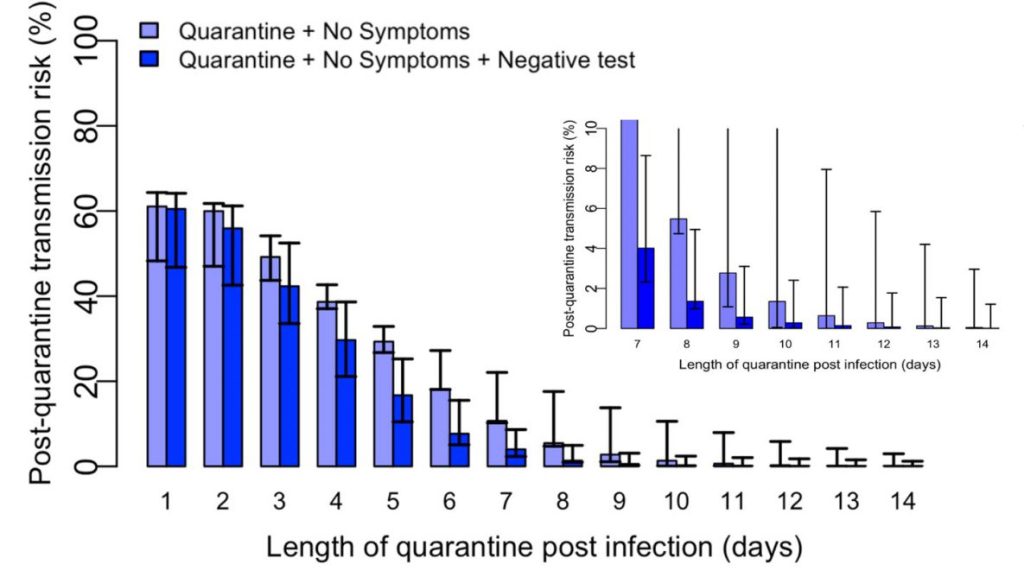
- The risk is near zero at day 14 which is consistent with data that motivated the initial 14-day recommendation.
- A negative test doesn’t make a difference until about day 5.
- There’s not a major change in the risk of transmission beyond day 10.
So I’m in the clear on day 10, right?
A very important thing the new recommendations highlight concretely is that exposed individuals are not completely in the clear after day 10. There is still a small but significant chance that they could show spread the infection up to day 14 (and even a bit beyond in very rare cases). If an exposed individual ends their quarantine on day 10 or earlier they still must monitor for symptoms closely up to day 14. This is not the time to assume a cough is an allergy or just a cold. Get tested if any symptoms develop. This is good advice even for those not in quarantine but this group has a higher risk of having the virus.
To sum it all up.
The CDC has used new modeling data to attempt to balance the risk of transmission with strategies to improve public compliance with its recommendations. The hope is that, even if there is slightly more transmission with a shorter quarantine on the individual level, increased compliance, on the whole, will more than compensate to bring total transmission down (or at least keep it the same with less misery on the part of the quarantined).
Their logic is sound but certainly up for debate. It is based on the major assumption that the new recommendations will improve compliance with quarantine recommendations. They do not cite any evidence that this will be the case, so I’m not sure how they know this will be true. If it is not true and shorter quarantine doesn’t increase compliance there could end being more transmission and community spread. I’m not personally knowledgeable or qualified enough to say their assumption is incorrect. If they are correct, and I pray they are, the burden of quarantine will be decreased and the pain of the pandemic will lessen a little for all of us. Wouldn’t that be novel…
The community is so appreciative that you keep us informed on the latest developments!!!
LikeLike
A thought provoking article that has me thinking about my own experience recovering on a COVID ward a couple of weeks ago. My abiding memory is seeing the suffering of those around me on Oxyflow and them CPAP. I was fortunate not to go in CPAP. It was so distresssing to see other patients pulling off their equipment as they could not cope…. witnessing some lose their battle.
In terms of quarantine, that poses different challenges. I completed mine and am so pleased to reconnect with the outside world again. I realised I had not been outside from 8th November (other than transit from hospital) until 3rd December. Whatever experts decide, I’m happy to comply with. Frankly, anything is better than the trauma of being on the ward with no visitors amongst the noise of chaos of it all. The saving grace was the tremendous care and love from the nurses for which I am eternally grateful and also the social media that allowed me to keep in contact with friends and recieve messages of support. Marty
LikeLike