This post will attempt to answer the following questions:
- What percentage of people who had COVID-19 produce neutralizing antibodies?
- What percentage of people who did not get tested but think they had COVID-19 produce antibodies.
- How long does it take to develop these antibodies?
I get regular calls from people asking questions about COVID-19. In the beginning of the pandemic these questions mainly centered around questions of who should get tested or seek medical advice. Over the past couple weeks the tenor has changed. Now the questions are more about coming out of quarantine. Many people tested positive or are assuming they were infected and now believe they are immune and are no longer abiding by the recommended recommendations of social distancing, hand washing, or mask wearing. I totally get it. I have regular transient mental breakdowns where I’m overwhelmed with the overwhelming weight of our current reality peppered with a sense that this is never going to end. I know that people are desperate to return to visiting relatives, leave their homes without anxiety, or just have an inkling of hope that this will all end at some point. It’s so much easier to overcome a challenging situation if you see the light at the end of the tunnel. Even if it’s going to be a long time, just knowing that there is an end to it all can ease anxiety greatly. So I get where it’s coming from but decisions that are made based on emotion alone rarely end well. This is always the case with medicine. Remember, the virus doesn’t care how sick of all this we are.
With that said, there has been recent news that is cause for optimisim. I have maintained and strongly believe that there is immunity after infection with COVID-19. Most infectious disease experts believe this to be true so I’m not a maverick here. This means that there will be an end to all this and that an understanding of the antibody response and the ability to test for it is the key to normalcy until an effective vaccine is developed (for the argument in support of this read here and here). There have been numerous antibody tests that have become available and people have been able to donate plasma which is more evidence supporting the fact that after recovery there is some level of protection from reinfection. The details are crucial here. We have seen that a few missteps and a few weeks delay can be disastrous. This is not the time to rely on opinions from social media. Now is the time for evidence. I believe there are two main questions that still need to be answered before this can be confirmed confidently enough to raise restrictions.
First, it is not clear what quantity of antibodies are necessary to confer immunity. It may be that some people mount only a weak immune response that does not produce enough antibodies to protect them from reinfection. This may relate to severity of their infection or be an intrinsic aspect of their immune system. This would mean people who were infected would be vulnerable to reinfection and to reigniting the pandemic. There is reason for caution. Many who have volunteered to donate plasma have been told they do not have sufficient antibodies to donate. In fact, one study of hospitalized patients showed that 36% had no or very weak antibody responses (and these were hospitalized patients!).
it is not clear what quantity of antibodies are necessary to confer immunity
Second, there are many people who have assumed they are infected with COVID-19 who actually weren’t. I know personally of cases where people were sure they were sick but tested negative. They assumed they were protected from reinfection which was not true. They would also be vulnerable to reinfection and spreading the virus.
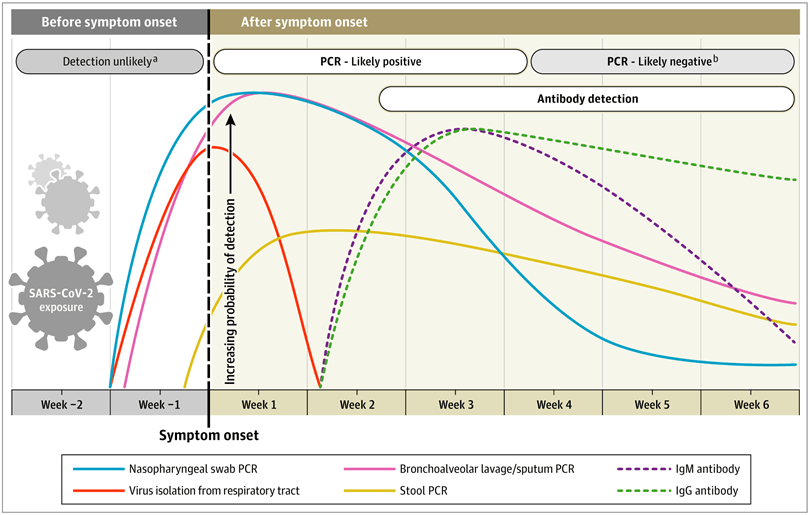
Third, the timing is not clear. How long does it take after you get sick before you have enough antibodies to be protected. There is likely a window between when you clear the virus and are immune. This was found in a recent JAMA article that documented the relationship of positive testing and antibody response over time. The main graph is at the top of the post. You can see there is a period of time where you cleared the virus (the red line) but haven’t produced enough antibodies (the dashed lines).
With all that said, there is hope. A recent preprint of an article that hopefully will be published soon analyzed the data from >1300 people who had completely recovered from COVID-19 and donated their plasma. The study documented antibody levels in this population. The patients volunteered and self reported whether they had COVID-19 but only about half were officially tested. The results were very interesting.
57 % of the group had a strong antibody response which is not a high number if you think about it. I’m not sure I would wager reigniting the pandemic on a coin flip. Fortunately, the study broke the groups down to those who tested positive and those who didn’t get a test but assumed they were positive.
First, the good news. For those who tested positive 82% developed a strong antibody response. Of the other 18%, 89% of those had increased titers on follow up testing. This means that about 98% of those who tested positive developed a strong antibody response eventually.
only 35% of the subjects who only thought they were sick and did not get tested had a strong antibody response
The bad news was that only 35% of the subjects who only thought they were sick and did not get tested had a strong antibody response. Remember, this was a population that were convinced enough that they had COVID-19 that they volunteered to donate their plasma. What this means is that there could be a significant population of people who are sure they were infected and are immune incorrectely and could get infected and recirculate the virus.
For those who tested positive about most had a strong antibody response by 3-4 weeks after symptom onset. This is important because you don’t want to test people too early or you may catch them in that window period I talked about above.
For those of you such as myself who have tested positive before we get too excited, remember that it is not known what levels of antibodies are necessary to protect from reinfection. It is also not known how long the antibodies stay at this level or if they decay and, if so, at what rate.
Also, remember that these data are from a well validated antibody test with very high accuracy and would not apply to tests that are not as well validated. There are a lot of unreliable tests out there so be careful drawing conclusions.
The bottom line:
- If you have tested positive and recovered you are likely immune but we don’t know what levels of antibody protect from reinfection or how long they last. Until this information becomes available people who tested positive should still take all the recommended precautions of social distancing, hand washing, and mask wearing (but with less anxiety).
- If you think you were sick but did not test positive or did not get tested at all, the odds are you are not immune. You might be but would need appropriate testing to confirm.
- The best time to get tested for antibodies is 3-4 weeks after the onset of symptoms.
Hopefully this information help bring a little light into this darkness. To me it means that we are closer to understanding who is immune and can return to normal function. It is a light at the end of the tunnel. We’re not at the end yet but its coming soon. Right now, I’ll take good news in any form.
dr Grove, thank you for this blog, it has and continues to be very helpful. Can you address sources of oxygen for patients who are hospitalized, ventilator vs Opti Flow or other methods and how they work. I have several relatives in NY, NJ and Detroit who ended up in ICU, one didnt make it, others are better or improving. I think i heard somewhere that being put on a ventilator can possibly cause more harm. My mother was put on Opti Flow and thank g-d she is out of the hospital and almost back to herself. I would love an explanation of the various forms of giving oxygen when a patient needs to be hospitalized. Thank you.
On Mon, May 11, 2020 at 1:57 PM My COVID Journey wrote:
> Dr. Grove posted: ” This post will attempt to answer the following > questions: What percentage of people who had COVID-19 produce neutralizing > antibodies?What percentage of people who did not get tested but think they > had COVID-19 produce antibodies. How long does it” >
LikeLike
I agree that ventilators may be a problem but not necessarily in all cases. See this post where I describe what I did a few weeks ago: https://mycovidjourney.com/2020/04/27/good-news-from-the-front-lines/
LikeLike
Dan:
Thanks for your continued updates!
Moshe
LikeLike
Thank you for sharing your journey and knowledge with us. As you know it’s hard to weed thru all the misinformation. I wanted to get your thoughts on a few things being someone we know and trust.
1. What are your thoughts on outdoor minyanim?
2. Does it make more sense to look at hospitalization numbers instead of just positive cases? My thought being that , atleast in Ohio, there has been a shortage of tests. They are planning on greatly increasing testing which will most likely lead to an increase in positive cases. These people are and have been walking around positive. If we watch hospital admissions would that give us a better idea of how the relaxed restrictions are affecting our area?
3. What are your thoughts on sleep away camp and day camps?
Hope you and family are well. Please give my regards to Chana.
Leah Shifrin
LikeLike
Any thoughts on the above questions? THank you
LikeLike
Is it possible that symptomatic people are testing NEGATIVE due to a mutation of the virus?
A relative of mine had a chest x-ray positive for pneumonia, followed by 2 weals of body aches and loss of smell/taste. She tested twice NEGATIVE for covid-19 (once at the time of the positive chest x-ray and again 2 weeks later when most of her symptoms resolved). She has not yet gotten antibody testing… It definitely seems, based on her symptoms, that she was covid-positive at some point…
But are the tests testing what they need to? Is it possible the virus mutated to a different strain and that’s why people like my relative above, who are clearly symptomatic, tested negative?
LikeLike
The mutation shouldn’t impact the PCR. It is more likely that she had false negative testing from improper technique.
LikeLike
Could not open this!
>
LikeLike
I double checked all the links and they all worked. Not sure the problem. Sorry for the trouble you had.
LikeLike
I was tested and have the antibody. Any new information about my immunity or if I can start going out.
LikeLike
The significance of antibody testing is not yet known so no conclusions can be drawn from a positive antibody test.
LikeLike